Infectious Diseases Case of the Month#17 |
|||
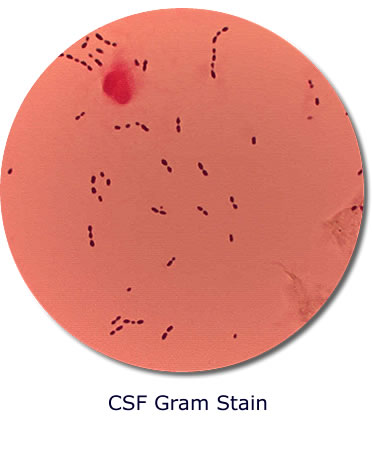 |
A 4 month-old white female infant was admitted to the hospital with meningitis. Four or five days prior to admission she had developed a low-grade fever without accompanying symptoms. Initially she seemed to improve but a couple days later developed higher fevers (101 to 103°) with fussiness but no cough, runny nose, etc. Subsequently she developed loose stools, vomiting, and lethargy. The day prior to admission she was seen in an urgent care facility where it was thought that she might have an ear infection. She was prescribed amoxicillin and ear drops. When seen by her pediatrician the following day she appeared lethargic and dehydrated. Her mother described having observed her infant's eyes "to roll back". On examination the child's temperature was 99.3°, her neck was supple, and although she appeared to have dry mucous membranes, her anterior fontanelle was bulging. She had no rash. Laboratory data included WBC 12.1, Hbg 9.6, and Plts 343. A lumbar puncture revealed these results: WBC 3250 (96% segmented neutrophils), glucose <3 mg/dl, and protein 197. CSF gram stain is at left. The infant had been previously healthy. She had received immunizations according to schedule including initial Haemophilus influenza type B and pneumococcal conjugate vaccines at age 2 mos. |
||
Which bacterium was the cause of this infant's meningitis? |
|||
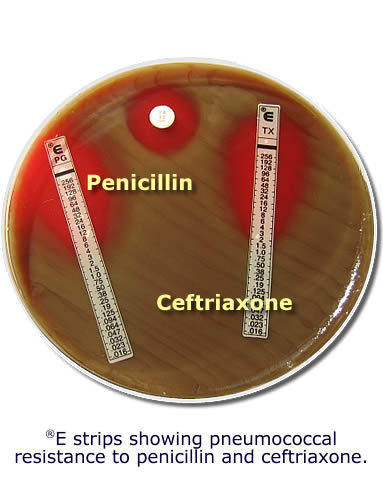 |
This child had meningitis secondary to drug resistant Streptococcus pneumoniae (DRSP). The child's CSF gram stain showed gram positive diplococci consistent with Streptococcus pneumoniae. She was begun on IV vancomycin and ceftriaxone as well as dexamethasone and by the following day showed clinical improvement. CSF cultures grew Streptococcus pneumoniae resistant to penicillin (MIC 4ug/ml) and ceftriaxone (MIC 2ug/ml) - see image at left. She continued to show clinical improvement and follow up CSF WBC on hospital days 3 and 6 were 1320/ul and 128/ul respectively. Blood cultures and subsequent CSF cultures were negative On the sixth hospital day she developed seizures necessitating anticonvulsant therapy and prompting transfer to a tertiary care children's hospital. There MRI scan showed no focal abnormality, and rifampin was added to her antimicrobial regimen. She did well clinically, completed 14 days of antimicrobial therapy, and returned home to her family thereafter apparently well (on anticonvulsant therapy). This case is interesting because of the presence of drug resistant Streptococcus pneumoniae (DRSP) as the cause of meningitis. The presence of both penicillin and ceftriaxone resistance makes therapy of invasive pneumococcal disease problematic. The potential for such resistance underlies recommendations for inclusion of vancomycin in empiric regimens for bacterial meningitis in both children and adults. The child in the described clinical vignette received therapy in conformance with the current recommendations of the American Academy of Pediatrics as outlined in the 2006 Red Book (including continued therapy with ceftriaxone despite resistance). Though dexamethasone therapy is of proven benefit in treatment of meningitis due to Haemophilus influenzae in children, its benefit in treatment of pneumococcal meningitis in children is still of some controversy particularly in cases of both ceftriaxone and penicillin resistance. Invasive pneumococcal disease including meningitis has become considerably less common in children since the introduction of pneumococcal conjugate vaccine (HCV7) in the United States in 2000 (see graphic). By 2003 the incidence of all invasive pneumococcal disease in children less than two years of age decreased by 80% and that due to vaccine and vaccine-related serotypes by approximately 90%. The infant in the case described had received her first dose of HCV7. That she developed meningitis with Streptococcus pneumoniae despite this relates either to incomplete immunity or infection with a non-vaccine strain serotype. The other bacteria listed amongst the choices in the preceding vignette (see original format) are potential causes of meningitis in children. Neisseria meningitidis is a gram negative diplococcus, Haemophilus influenzae is a gram negative coccobacillus, and Listeria monocytogenes is a gram positive rod. Streptococcus agalactiae (Group B Strep) is a gram positive coccus that would be very difficult to distinguish from Streptococcus pneumoniae on gram stain. However, it would be very unlikely to cause meningitis in children beyond the neonatal stage. Ref: Red Book - 2006 Report of the Committee on Infectious Diseases, American Academy of Pediatrics |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||